Follicle Stimulating Hormone: Low vs High Signs, Testing, Ovulation, and Fertility
Overview
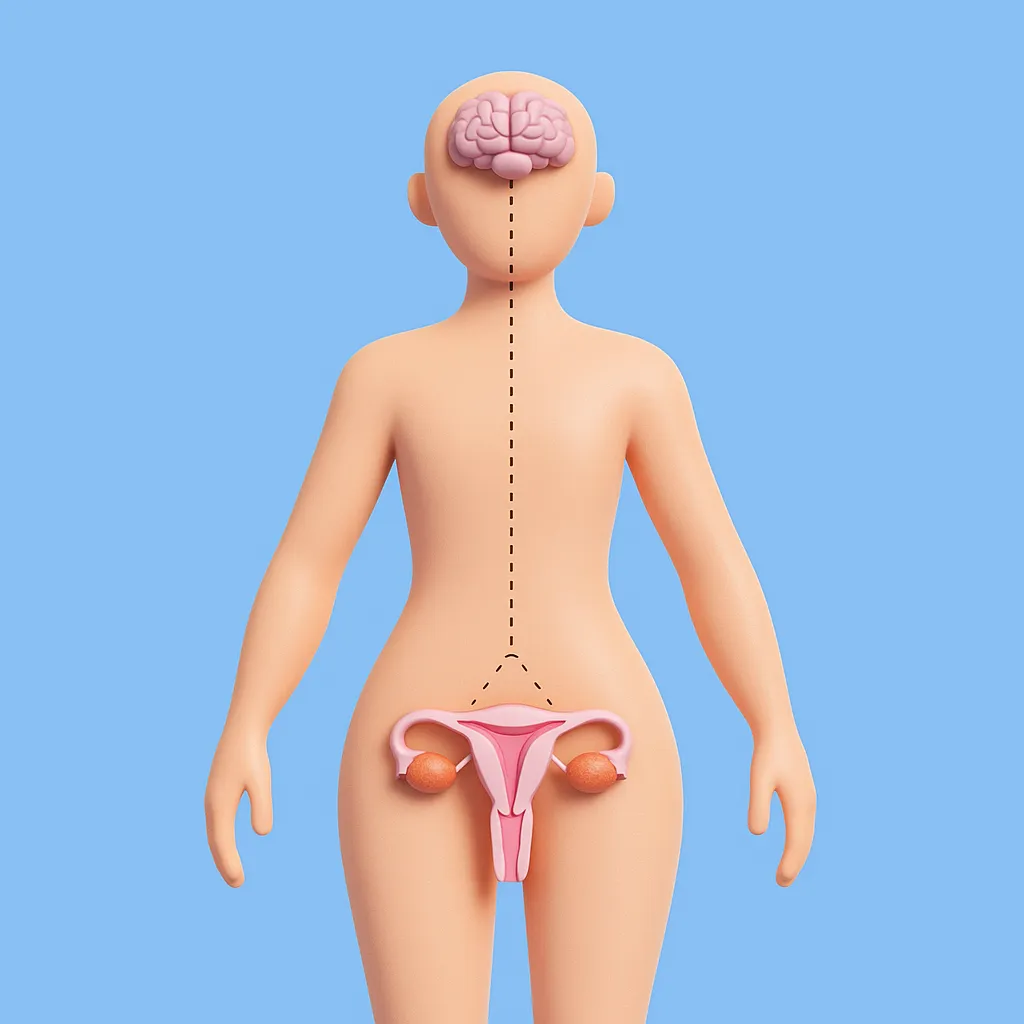
Follicle stimulating hormone, usually shortened to FSH, is a pituitary hormone that supports egg development and ovulation in women and sperm production in men. In the ovaries it helps follicles grow and prepare for an egg to be released. In the testes it works with other signals to support sperm making cells. FSH is a core marker in many fertility and cycle evaluations.
Clinicians almost always interpret FSH together with Luteinizing Hormone and sex hormones, because the pattern between them tells more than any single number.
What Follicle Stimulating Hormone is and where it is made
FSH is a peptide hormone produced by the pituitary gland at the base of the brain.
Its release is driven by gonadotropin releasing hormone from the hypothalamus and tuned by feedback from estrogen, progesterone, and testosterone.
FSH travels through the bloodstream to the ovaries in women and the testes in men, where it acts on specific target cells.
What Follicle Stimulating Hormone does in your body
Stimulates ovarian follicles to grow and mature before ovulation.
Helps set up the follicle that will respond to the luteinizing hormone surge and release an egg.
Supports estrogen production in the first half of the menstrual cycle.
In men, works with luteinizing hormone to support sperm production in the testes.
Contributes to overall fertility, cycle regularity, and sex hormone balance.
When testing Follicle Stimulating Hormone makes sense
Irregular, very long, or very short menstrual cycles, or periods that stop without clear reason.
Difficulty conceiving when cycle tracking suggests possible ovulation issues.
Evaluation of suspected polycystic ovary syndrome together with symptoms, ultrasound, and other hormones.
Assessment of ovarian reserve in some fertility workups, usually along with age and other tests.
Suspected early menopause or primary ovarian insufficiency.
Evaluation of low testosterone and fertility concerns in men, to help distinguish testicular from pituitary causes.
Workup of early or delayed puberty in children and adolescents.
How to think about high and low Follicle Stimulating Hormone results
This information is general and does not replace lab specific reference ranges, cycle timing, or medical evaluation.
Low FSH might be associated with:
Lack of ovulation, irregular or absent periods, and reduced fertility in women when sex hormone levels are also low.
Low testosterone with low or inappropriately normal FSH in men, suggesting a pituitary or hypothalamic cause.
Delayed puberty when both FSH and sex hormones are below expected levels for age.
Possible contributors include hypothalamic amenorrhea from underfueling or high stress, pituitary or hypothalamic disease, some systemic illnesses, and long term use of hormonal medications that suppress the reproductive axis.
High FSH might be associated with:
Menopause and primary ovarian insufficiency, where the ovaries are less responsive and FSH rises in compensation.
Reduced ovarian reserve in some fertility evaluations, particularly when high for age and life stage.
Primary testicular failure in men, where the testes do not respond well and FSH is elevated.
Normal mid cycle changes when interpreted in the correct cycle window.
Markedly high FSH can also be seen with some genetic and gonadal conditions. Interpretation always depends on age, sex, cycle phase, and partner labs such as luteinizing hormone, estrogen, progesterone, and testosterone.
What can influence your Follicle Stimulating Hormone levels
Menstrual cycle phase and whether ovulation is approaching or has occurred.
Age and life stage, including puberty, reproductive years, and menopause.
Ovarian reserve and testicular health, including prior surgery, radiation, or chemo.
Energy availability, body weight, and training load, especially in hypothalamic amenorrhea.
Chronic stress and systemic illness that can alter hypothalamic and pituitary signals.
Hormonal contraception, fertility medications, and other hormone therapies.
Pituitary and hypothalamic health, including benign tumors, prior surgery, trauma, or radiation.
When to talk to a clinician about Follicle Stimulating Hormone
FSH results that are clearly outside the reference range and do not match your age or life stage.
Persistent irregular cycles, missed periods, or difficulty conceiving.
Symptoms that suggest early menopause or primary ovarian insufficiency, such as long gaps between periods or hot flashes at a younger age.
Low libido, fertility concerns, or low testosterone in men.
Concerns about early or delayed puberty in children or adolescents.
A clinician can interpret FSH alongside luteinizing hormone, sex hormones, imaging, and your history to decide whether watchful waiting, lifestyle changes, more testing, or treatment is appropriate.
Follicle Stimulating Hormone in one view
Follicle stimulating hormone is a pituitary signal that helps grow ovarian follicles and support sperm production, making it central to ovulation, fertility, and sex hormone balance. On its own the number is hard to use, so FSH is most helpful when timed correctly and read together with Luteinizing Hormone and key sex hormones such as Estrogen. If your FSH is outside range or does not match your symptoms or life stage, it is a good reason to discuss the full pattern with a clinician instead of trying to interpret or treat it in isolation.